X-ray of hip prostheses

Author:
Mikael Häggström [notes 1]
For X-ray of the hip joint in the presence of a prosthesis, this article first deals with the first postoperative image which is more focused at prosthesis configuration, and separately describes subsequent follow-ups which are more focused at complications.
Contents
Quality checking
- The referral or complementary information needs to specify the type of prosthesis and when it was inserted.[2]
- Images that need to be available include the first postoperative ones, as well as the most recent previous exam.[2]
First postoperative image: Configuration
Post-operative projectional radiography ("X-ray") is routinely performed to ensure proper configuration of hip prostheses.
The direction of the acetabular cup influences the range of motion of the leg, and also affects the risk of dislocation.[3] For this purpose, the acetabular inclination and the acetabular anteversion are measurements of cup angulation in the coronal plane and the sagittal plane, respectively.
Acetabular anteversion.[5] This parameter is calculated on a lateral radiograph as the angle between the transverse plane and a line going through the (anterior and posterior) margins of the acetabular cup.[5]
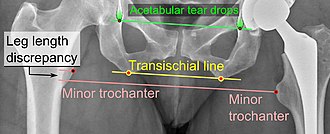
Center of rotation: The horizontal center of rotation is calculated as the distance between the acetabular teardrop and the center of the head (or caput) of the prosthesis and/or the native femoral head on the contralateral side.[4] The vertical center of rotation instead uses the transischial line for reference.[4] The parameter should be equal on both sides.[4]
Cement coverage is regarded as acceptable when there are no translucent zones on an anteroposterior image in at least 6 of 7 Gruen-zones.[2] Absence of cement in zone 7 (medially-proximally) needs to be noted. On a lateral image, the distal tip of the prosthesis should be centered, and not be in contact with the cortex.[2] The cup should not have translucent zones in zone 1 and 2. It is acceptable to have translucent zones in parts of zone 3.[2]
Report
The postoperative report should include:[2]
- Prosthesis configuration. If the report is likely to undergo double reading, the parameters need to be given in numbers even if within normal limits.
- Cement coverage.
- See also: General notes on reporting
Further follow-ups: Complications
Further follow-ups after the initial postoperative image are focused on various complications.
Dislocation
Fracture
Post-operative femoral fractures are graded by the Vancouver classification:
| Type | Description |
|---|---|
| A | Fracture in the trochanteric region |
| B1 | Fracture around stem or just below, with well fixed stem |
| B2 | Fracture around stem or just below, with loose stem but good proximal bone |
| B3 | Fracture around stem or just below, with poor quality or severely comminuted proximal bone |
| C | Fracture below theprosthesis |
Loosening
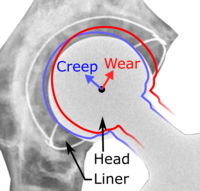
On radiography, it is normal to see thin radiolucent areas of less than 2 mm around hip prosthesis components, or between a cement mantle and bone. However, these may still indicate loosening of the prosthesis if they are new or changing, and areas greater than 2 mm may be harmless if they are stable.[9] The most important prognostic factors of cemented cups are absence of radiolucent lines in DeLee and Charnley zone I, as well as adequate cement mantle thickness.[10] In the first year after insertion of uncemented femoral stems, it is normal to have mild subsidence (less than 10 mm).[9]
Report
Further follow-up reports should include at least:
- Dates of the images used for comparison
- Absence of change in position, or a description of any change.[2]
- Absence or of loosening, or a description of it.[2]
- See also: General notes on reporting
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Radlines:Authorship for details.
References
- ↑ Andrew Still (2002-11-02). Total Hip Replacement. University of Southern California. Retrieved on 2017-01-05.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Radiologists: Torsten Boegård, Mats Geijer, Marianne Petrén-Mallmin. Orthopedic surgeons: Lennart Sanzén, Christer Strömberg, Torbjörn Ahl. Hip - Radiologic evaluation of prosthetic surgery (Swedish title: HÖFT - Radiologisk undersökning vid proteskirurgi). Swedish Orthopaedic Association (SOA). Publication #18, 2006
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Iain Watt, Susanne Boldrik, Evert van Langelaan and Robin Smithuis. Hip - Arthroplasty -Normal and abnormal imaging findings. Radiology Assistant. Retrieved on 2017-05-21.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Vanrusselt, Jan; Vansevenant, Milan; Vanderschueren, Geert; Vanhoenacker, Filip (2015). "Postoperative radiograph of the hip arthroplasty: what the radiologist should know ". Insights into Imaging 6 (6): 591–600. doi:. ISSN 1869-4101. PMID 26487647.
- ↑ 5.0 5.1 Shin, W. C.; Lee, S. M.; Lee, K. W.; Cho, H. J.; Lee, J. S.; Suh, K. T. (2015). "The reliability and accuracy of measuring anteversion of the acetabular component on plain anteroposterior and lateral radiographs after total hip arthroplasty ". The Bone & Joint Journal 97-B (5): 611–616. doi:. ISSN 2049-4394.
- ↑ John J. Callaghan, Aaron G. Rosenberg, Harry E. Rubash (2007). The Adult Hip, Volume 1 . Lippincott Williams & Wilkins. p. 958. ISBN 978-0-7817-5092-9.
- ↑ Neumann, Daniel R.P.; Thaler, Christoph; Hitzl, Wolfgang; Huber, Monika; Hofstädter, Thomas; Dorn, Ulrich (2010). "Long-Term Results of a Contemporary Metal-on-Metal Total Hip Arthroplasty ". The Journal of Arthroplasty 25 (5): 700–708. doi:. ISSN 0883-5403.
- ↑ Daniel J. Berry, Jay Lieberman (2012). Surgery of the Hip . Elsevier Health Sciences. p. 1035. ISBN 9781455727056.
- ↑ 9.0 9.1 Roth, Trenton D.; Maertz, Nathan A.; Parr, J. Andrew; Buckwalter, Kenneth A.; Choplin, Robert H. (2012). "CT of the Hip Prosthesis: Appearance of Components, Fixation, and Complications ". RadioGraphics 32 (4): 1089–1107. doi:. ISSN 0271-5333.
- ↑ Steffen Breusch, Henrik Malchau (2005). The Well-Cemented Total Hip Arthroplasty: Theory and Practice . Springer Science & Business Media. p. 336. ISBN 978-3-540-24197-3.