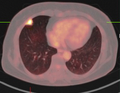
CT of lung nodules
Authors:
Mikael Häggström; Authors of integrated Creative Commons article[1] [notes 1]
A lung nodule or pulmonary nodule is a relatively small focal density in the lung. This article deals with the presence a solitary pulmonary nodule (SPN) or coin lesion, which is a mass in the lung smaller than 3 centimeters in diameter.[2]
Contents
Scope
The content may be applied to the presence of a few solitary pulmonary nodules, each of which is defined as a single lesion in the lung completely surrounded by functional lung tissue with a diameter less than 3 cm, and without associated pneumonia, atelectasis (lung collapse) or lymphadenopathies.[3][4]
Planning
Choice of investigation
- CT of lung nodules is the modality of choice for reevaluating solitary pulmonary nodules visible on X-ray of the thorax, and for subsequent monitoring.[5]
Evaluation
Always evaluate the following:
- Size: larger size confers a higher risk of cancer[6]

- Location: Upper lobe location is a risk factor for cancer, while a location close to a fissure or the pleura indicates a benign lymph node,[6] especially if having a triangular shape.[1]
- Margin morphology: a spiculated margin is a risk factor for cancer.[6] Benign causes tend to have a well defined border, whereas lobulated lesions or those with an irregular margin extending into the neighbouring tissue tend to be malignant.[4] In particular, spiculations are highly predictive of malignancy with a positive predictive value up to 90%.[1] Also, a "notch sign", which is an abrupt indentation of the nodule, increases the risk of cancer, but may also be found in granulomatous diseases.[1]
Round well-delineated solid lung nodule with smooth border.[1]
Lobulated nodule.[1]
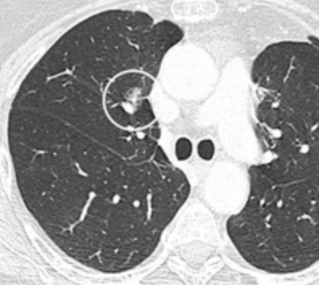
Spiculated lung nodule.[1]
A "notch sign".[1]
A triangular perifissural node can be diagnosed as a benign lymph node.[1]
- Multiplicity: Where the presence of up to an additional 3 nodules has been found to increase the risk of cancer, but decrease in case of 4 or more additional ones, likely because it indicates a previous granulomatous infection rather than cancer.[6]
- Presence of emphysema and/or lung fibrosis, which are risk factors for cancer.[6]
- Enhancement: If the exam is done as a combined non-contrast and contrast CT, a solitary nodule with an enhancement off less than 15 Hounsfield units (HU), whereas a higher enhancement indicates a malignant tumor (with a sensitivity estimated at 98%).[7]

- Areas of fatty tissue (−40 to −120 HU) indicates a hamartoma. However, only about 50% of hamartomas are fat containing.[1]
If previous exams are available, also evaluate:
- Growth rate: solid cancers generally doubles in volume over between 100 to 400 days, while subsolid cancers (generally representing adenocarcinomas) generally doubles in volume over 3 to 5 years.[6] One volume doubling equals approximately a 26% increase in diameter.[6] In comparison, the typical size doubling are less than 20 days for infections, and more than 400 days for benign nodules.[8]
Preferably also look for the following signs:
- If there is a central cavity, then a thin wall points to a benign cause whereas a thick wall is associated with malignancy (especially 4 mm or less versus 16 mm or more).[4]
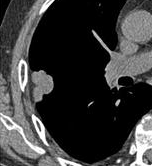
Cavitation with relatively thick wall, in this case aspergilloma).[1]

- In case of calcifications, a popcorn-like appearance indicates a hamartoma, which is benign.[9]
- In case of subsolid nodules, being part solid has a higher risk of cancer than being purely ground glass opacity.
Part solid nodule.[1]
Ground glass opacity nodule.[1]
- Pleural retraction is far more common in cancers.[1] It is the pulling of visceral pleura towards the nodule.[1]
Nodule with pleural retraction.[1]
In this case, pleural retraction is seen as a triangular fat component.[1]

- A lung nodule abutting a pulmonary cyst is a rare finding, yet indicating cancer.[1]
- Bubble-like lucencies in the nodule indicate cancer:[1]

- Vascular convergence is where vessels converge to a nodule without adjoining or contacting the edge of the nodule, and is mainly seen in peripheral subsolid lung cancers.[1] It reflects angiogenesis.[1]
Air bronchograms is defined as a pattern of air-filled bronchi on a background of airless lung, and may be seen in both benign and malignant nodules, but certain patterns thereof may help in risk stratification.[1]
- Further information: Air bronchogram
CT densitometry, measuring absolute attenuation on the Hounsfield scale, has low sensitivity and specificity and is not routinely employed, apart from helping to distinguish solid from ground glass lesions, and to confirm visible fatty areas or calcifications.[7]
Further management
Further management depends largely on an overall radiologic classification of a nodule as low or high cancer risk, which is rather subjective. Furthermore, it generally also requires knowledge of general risk factors of cancer (such as exposure to tobacco smoking or other carcinogens such as asbestos, previously diagnosed cancer, respiratory infections, or chronic obstructive pulmonary disease.[10]). For incidentally detected nodules on CT scan, Fleischner Society guidelines are given in table below. For multiple nodes, management is based on the most suspicious node.[6] These guidelines do not apply in lung cancer screening, in patients with immunosuppression, or in patients with known primary cancer.[6]
| <6 mm (<100mm3) | 6-8mm (100-250mm3) | >8mm (>250mm3) | ||
|---|---|---|---|---|
| Single nodule |
Low risk | No routine follow-up | CT after 6-12 months, then consider CT after 18-24 months | Consider CT at 3 months, PET-CT or biopsy |
| High risk | Optionally, CT after 12 months | CT after 6-12 months, then after 18-24 months | ||
| Multiple nodules |
Low risk | No routine follow-up | CT after 3-6 months, then consider CT after 18-24 months | |
| High risk | Optionally CT after 12 months | CT after 3-6 months, then after 18-24 months | ||
| Total size <6 mm (<100mm3) | Total size >6mm (>1003) | ||
|---|---|---|---|
| Single nodule |
Ground glass opacity | No routine follow-up | CT after 6-12 months to check if persistent, then after 2 years and then another 2 years |
| Part solid | No routine follow-up | CT after 6-12 months:
|
|
| Multiple nodules |
CT after 3-6 months. If stable, consider CT after 2 and then another 2 years. | CT after 3-6 months, then after 18-24 months | |
More frequent CT scans than what is recommended has not been shown to improve outcomes but will increase radiation exposure and the unnecessary health care can be expected to make the patient anxious and uncertain.[11]
- PET scan

If there is an intermediate risk of malignancy, further imaging with positron emission tomography (PET scan) is appropriate (if available). It can be done as a PET-CT. Around 95% of patients with a malignant nodule will have an abnormal PET scan, while around 78% of patients with a benign nodule will look normal on PET (this is the test sensitivity and specificity).[12] Thus, an abnormal PET scan will reliably pick up cancer, but several other types of nodules (inflammatory or infectious, for example) will also show up on a PET scan. If the nodule has a diameter of less than one centimeter, PET scans are often avoided because of an increased risk of falsely normal results.[12][13][14] Cancerous lesions usually have a high metabolism on PET, as demonstrated by their high uptake of FDG (a radioactive sugar).
Notes
- ↑ For a full list of contributors, see article history. Creators of images are attributed at the image description pages, seen by clicking on the images. See Radlines:Authorship for details.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 Snoeckx, Annemie; Reyntiens, Pieter; Desbuquoit, Damien; Spinhoven, Maarten J.; Van Schil, Paul E.; van Meerbeeck, Jan P.; Parizel, Paul M. (2017). "Evaluation of the solitary pulmonary nodule: size matters, but do not ignore the power of morphology ". Insights into Imaging 9 (1): 73–86. doi:. ISSN 1869-4101.
- ↑ . Coin lesion (Lung).
- ↑ Tan BB, Flaherty KR, Kazerooni EA, Iannettoni MD; Flaherty; Kazerooni; Iannettoni; American College of Chest Physicians (January 2003). "The solitary pulmonary nodule ". Chest 123 (1 Suppl): 89S–96S. doi:. PMID 12527568. Archived from the original. .
- ↑ 4.0 4.1 4.2 Winer-Muram HT (April 2006). "The solitary pulmonary nodule ". Radiology 239 (1): 34–49. doi:. PMID 16567482. Archived from the original. .
- ↑ "Evaluation of the solitary pulmonary nodule ". Am Fam Physician 80 (8): 827–31. October 2009. PMID 19835344.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 MacMahon, Heber; Naidich, David P.; Goo, Jin Mo; Lee, Kyung Soo; Leung, Ann N. C.; Mayo, John R.; Mehta, Atul C.; Ohno, Yoshiharu; et al. (2017). "Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017 ". Radiology 284 (1): 228–243. doi:. ISSN 0033-8419.
- ↑ 7.0 7.1 Tanay Patel. Lung Metastases Imaging. Medscape. Updated: Sep 30, 2018
- ↑ Truong, MD, Mylene T.; Ko, MD, Jane P.; Rossi, MD, Santiago E.; Rossi, MD, Ignacio; Viswanathan, MD, Chitra; Bruzzi, MBBCh, John F.; Marom, MD, Edith M.; Erasmus, MD, Jeremy J. (2014). "Update in the Evaluation of the Solitary Pulmonary Nodule ". Radiological Society of North America 34 (6): 1658–1679. doi:. PMID 25310422.
- ↑ Ost D, Fein AM, Feinsilver SH; Fein; Feinsilver (June 2003). "Clinical practice. The solitary pulmonary nodule ". N. Engl. J. Med. 348 (25): 2535–42. doi:. PMID 12815140.
- ↑ Zhan, Ping; Xie, Haiyan; Xu, Chunhua; Hao, Keke; Hou, Zhibo; Song, Yong (2013). "Management strategy of solitary pulmonary nodules ". Journal of Thoracic Disease 5 (6): 824–829. doi:. PMID 24409361.
- ↑ American College of Chest Physicians; American Thoracic Society (September 2013). "Five Things Physicians and Patients Should Question
". Choosing Wisely: An Initiative of the ABIM Foundation (American College of Chest Physicians and American Thoracic Society). Archived from the original. . Retrieved on 6 January 2013Template:Inconsistent citations, which cites
- Smith-Bindman, R; Lipson, J; Marcus, R; Kim, KP; Mahesh, M; Gould, R; Berrington de González, A; Miglioretti, DL (Dec 14, 2009). "Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer.
- Wiener, RS; Gould, MK; Woloshin, S; Schwartz, LM; Clark, JA (Mar 2013). "What do you mean, a spot?: A qualitative analysis of patients' reactions to discussions with their physicians about pulmonary nodules.
- ↑ 12.0 12.1 Gould MK, Maclean CC, Kuschner WG, Rydzak CE, Owens DK; MacLean; Kuschner; Rydzak; Owens (February 2001). "Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis ". JAMA 285 (7): 914–24. doi:. PMID 11180735. Archived from the original. .
- ↑ Khan A (March 2007). "ACR Appropriateness Criteria on solitary pulmonary nodule ". J Am Coll Radiol 4 (3): 152–5. doi:. PMID 17412254. Archived from the original. .
- ↑ Vansteenkiste JF, Stroobants SS; Stroobants (January 2006). "PET scan in lung cancer: current recommendations and innovation ". J Thorac Oncol 1 (1): 71–3. doi:. PMID 17409830.